Understanding polymicrobial interactions
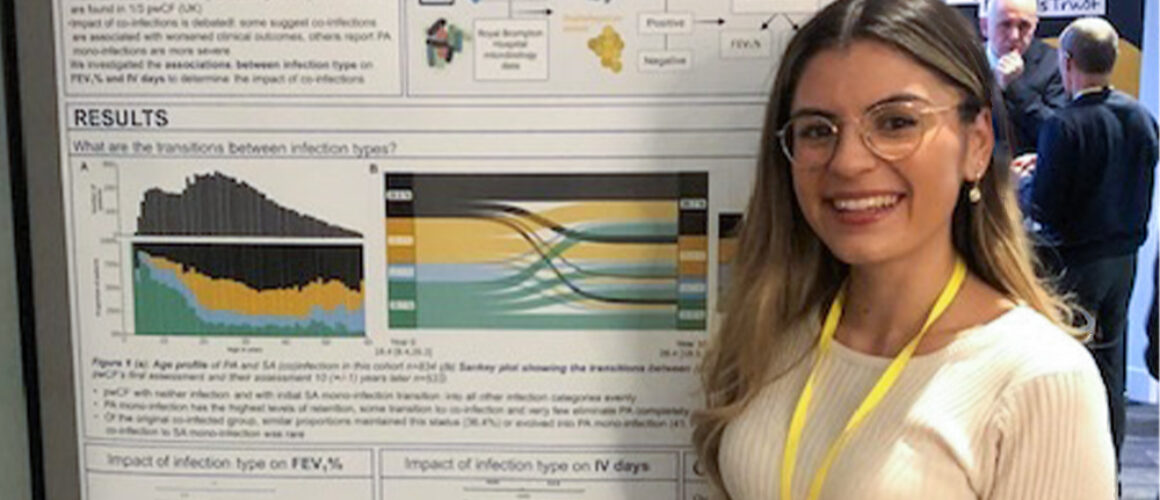
Micaela is a PhD student based at Imperial College London. Her research is focused on Staphylococcus aureus and Pseudomonas aeruginosa co-infections in Cystic Fibrosis. Micaela is supervised by Professor Jane Davies and Dr Laura Nolan and is part of a group of academics based at one of the Strategic Research Centres funded by the Cystic Fibrosis Trust. We caught up with Micaela to find out more about her research.
Micaela, can you tell us a little about the work you are doing- what were the challenges you are trying to address?
My PhD research is about gaining a deeper understanding of the relationships between the two most common bacterial infections in CF – Pseudomonas aeruginosa and Staphylococcus aureus. It is known that Pseudomonas aeruginosa is a problem bug for people with CF, but infections in people with CF infections are polymicrobial in nature, meaning that there are multiple species of bacteria and fungi present in the lung at the same time. These different microorganisms can work together or against each other, and this is thought to have beneficial or detrimental effects on the person with CF. It’s important to uncover the underlying mechanisms that drive these interactions, as they are thought to play a role in the health and well-being of people with CF.
And what might be the implications of your research on the management of infections in people with CF?
My goal is to find out more about these microbial interactions, to help to inform clinical teams about how to treat people with CF. With more information about these bugs, they can choose the right treatment that will be the most effective for each person. For example, some antibiotics are known to be less effective if there are multiple species of bacteria present as they can interact to become resistant to the treatments. As we aim for treatment to become more personalised, taking this into consideration could become more important to improve the management of infections.
Research-wise, what are your next steps?
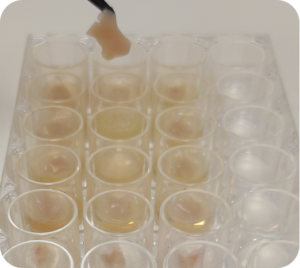
I am currently about to begin the last year of my PhD. I’m really enjoying the new microscopy techniques I’m learning, which enable us to see and image bacteria using a microscope, and I hope to develop them further over the next year. I am planning to hand in my thesis by the end of 2024 and apply for postdoctoral research positions where I hope to continue studying polymicrobial interactions.
How did you get into CF anti-microbial research, and why do you find it so interesting?
I really wanted to study something that had translational potential, where findings could directly benefit people. CF really stood out to me as infection continues to pose challenges despite the new modulator therapies. The James Lind Alliance, a priority setting initiative, that brings patients, carers and clinicians together has repeatedly highlighted infection treatment as a priority in CF. Contributing to the understanding of something that is clearly a priority to everyone in the CF community is really meaningful to me, particularly as I have half siblings with CF.
As a microbiologist, infection in CF is also incredibly important as it provides a unique opportunity to understand and tackle chronic infection. There are unique adaptations that bacteria undergo when infection becomes chronic, like increases in antibiotic resistance. How bacteria are able to adapt to the lung environment and the presence of other species over time is my specific interest as understanding these adaptations is key to enable us to tackle infections and treat them effectively.
How important is collaboration in your work? Are there any areas of research/capabilities in particular that you’re looking to collaborate in?
Collaboration has been so important in my PhD so far. In Prof Davies’ lab, I’ve been incredibly lucky to work with both doctors and scientists which has given me a unique insight into CF research. It has taught me how important it is to collaborate in our work so that we keep research focused and tailor it so that it is beneficial to the clinical teams who will be the ones to implement any findings.
I have also had a great opportunity to work on an infection dataset with a statistician, Dr Jonathan Ish-Horowicz, who was able to help us to use the statistics that we needed to unlock the potential of this dataset. This data is now being used by more data analysts at LifeArc to help us understand the associations between different infection types and the health of people with CF. Having their expertise to work on this project is so incredibly valuable and allows work like this to happen and hopefully for it to have an impact in the clinic in the future.
I’m always looking to learn more techniques that could be useful in my work, and I have been so lucky to have amazing teams around me who have been willing to teach me. For that I would like to thank Dr Martin Welch and his lab in Cambridge University, who have always welcomed me into their lab to learn their techniques, as well as Dr Andrew Edwards’ lab in Imperial College and Prof Andy Bush from the Royal Brompton Hospital, who have advised me as my internal examiners and also kindly shared their expertise. Currently, I am a visiting student at the Quadram Institute, working closely with Prof Cynthia Whitchurch’s lab as well as my supervisor Dr Laura Nolan, who have gone above and beyond to teach me about microscopy and imaging biofilms but more importantly how to have fun in the lab and have reminded me why being a scientist is one of the greatest jobs in the world!
Last but not least, I am incredibly and sincerely thankful to the CF Trust for funding this work, recognising its importance as well as working together with scientists so that people with CF can live a life unlimited.
If you want to follow Micaela and stay up to date with her research, follow her on social media (Instagram or X/Twitter)








 We caught up with Dr Sam Westgate, CEO of
We caught up with Dr Sam Westgate, CEO of